Overcoming “Chronic Disease Persona”
In a few short weeks, I reach another milestone-my 50th birthday. I’m a firm believer that age is just a number. I’ve seen people younger than me who look like they are older, and elderly people who look much younger than their age.
That belief hasn’t been so firm over the past month.
I’ve had hereditary neuropathy (Charcot Marie Tooth or CMT) all of my life, but it wasn’t until around 1996 that I found out about my PKD (Polycystic Kidney Disease). Around 2003, my kidney function went below 60% (the magic cutoff for Stage III CKD, or Chronic Kidney Disease). It was probably at that point that I started with, as I call it, the “Chronic Disease Persona”.
Having been a nurse for 24 years, I’ve seen a wide spectrum of how people react to their chronic illness. This includes denial, anger, acceptance, and the other extreme of letting it consume their life either to the point of becoming so fixated that they try whatever they can to fix it, or they become depressed and hopeless. For me, I was more towards the acceptance part of the spectrum, with a brief period of looking for fixes that just aren’t there.
I’m a very analytical person; my mind works constantly to figure out specific problems (not the math type either), and come up with plans and solutions. I’ve been through a fair amount since 2005, when my GFR hit the magic 20%; you know, the time they tell you that you need a dialysis fistula, and “let’s get you evaluated for the transplant list”. In August 2005, I had surgery to “create” my dialysis fistula, and less than a month later, emergency brain surgery for a subdural hematoma, followed several days later with seizures, and a hospitalization. Since then, I’ve had my transplant, major surgery on both feet to “reconstruct them” (by far the most painful of the 8 surgeries, but worth it), and several other “speed bumps” along the way.
It probably wasn’t until around 2005 that my “Chronic Disease Persona” was at full bore. But it took my upcoming birthday to realize that the birthday isn’t what is affecting me. It’s the fact that I have been looking at myself as someone who has a lot of medical issues. And that just isn’t me. I try to live the phrase “it is what it is”, and I think I have been doing that fairly well. Overall, I’ve done my best not to let my illnesses consume my life, but ironically, they’ve been doing that lately, even though I’m in MUCH better shape now than in 2005! So with that realization, I’ve decided it’s time to drop the CDP and think of myself as normal (although that’s a relative term). Back to enjoying life-playing practical jokes at work (which I was famous for), laughing more, enjoying family and friends once again.
It’s easy to slip into CDP. Those of us with chronic illnesses have more contact with the healthcare system; labs, doctor visits, procedures, tests, none of which we really have any control over. But it’s how we react to all of this that really matters. Although we may do our best to deal with it, I think that without realizing it, it affects us.
Now that I have realized this, I’ve decided to return to how I was (at least mentally/emotionally) before the rollercoaster ride began in 2005. I’ve had fixed what needed to be fixed, and there are FINALLY no upcoming surgeries on the horizon.
Under the guise of the “crisis” of turning 50, I had my ear repierced this past weekend. I had it pierced back in the mid 90′s, and kept the earring in until around 2005, when a lot of this started. So for me, it’s really symbolic-it’s my way of becoming “normal” again. My initial thought on doing it was that I was turning 50 soon, and was a way of fighting this. But now that I think of it, I really think it’s more of a fight against how I was living, thinking of myself as a “chronic”.
So take some time to think about how YOU are dealing with your chronic disease. Make changes; it’s easy to get “stuck” in all that we must deal with. Small changes can make a big difference.
Slip up
“Chronic disease with a positive attitude”. While I came up with that on my own, there is a definite basis for it.
In the 15 years and 8 months of MY life that my mother was alive, that is how she lived. I never knew my mother to be healthy. She walked in to my Middle School band concert using a cane (she was in her early 30’s at the time), it was not unusual for her to spend a month at a time in the hospital, and she’d be nauseated and tired between dialysis treatments up until it was the morning of dialysis, when she would then start the vicious cycle all over after her dialysis treatment.
Lately though, I haven’t exactly been following this example. The first part of the subtitle is one which I have no control over-“chronic disease”, but the last part, “with a positive attitude”, I one which I do have a LOT of control. Without going into too much detail, work and life stressors consumed me, and anxiety and sleeplessness were my way of life for the past few months. But that has resolved; I’m now able to sleep the entire night, and the anxiety is pretty much gone. A much needed vacation from my full time job did the trick (amongst other things). I have tons of vacation time, but I try to keep a “cushion” for any unforeseen health crisis, of which I’ve had several since 2005. I learned my lesson (we continue to learn until the day we die, I suspect). With 50 vacation days (which remain after last weeks vacation), I can afford to take more than what I’ve been taking, and taking 4 weeks off to recover from major surgery does NOT count as vacation. I’ve also had some job disappointments lately, but I can attest to the fact that when one door closes, another opens. It’s happened once, and as of today, will probably be happening again in the very near future.
Getting back to my Mom, she was truly my inspiration. I didn’t realize that at the time, but I do now. And I’ve tried my best to set the same example for my son, who may some day face some of the hurdles I have faced.
I accept the fact that I’ll never be able to do the physical things I’d like to do, like be able to jog, play baseball, or be able to go up and down steps without holding on to a railing. But that doesn’t mean I can’t do other things. From the time I was young, I’ve compensated for this by developing my mind, and I think I’ve done a pretty good job at that.
I’m fortunate to have made the career change from teacher to nursing, because over the past 27 years in healthcare (24 as a nurse), I’ve seen a lot worse than I’ve had to deal with, which has given me a unique perspective, something that not all people with a chronic illness have had the opportunity to experience.
The point of all of this is, that in dealing with chronic illness (or even the sudden onset of an acute illness), either as the “patient” or as a family member, it’s important to stay positive, while being realistic. I firmly believe that in order to maintain a stable state of health, much of the “battle” is to maintain a positive state of mind. Another point is that there may be things you can’t do, but there are things you CAN do. Take a chance. Sure, it’s scary making a major life change-as humans, change is difficult. But don’t look at the negatives; rather, think of the positives. You’re comfortable in your job, but will you regret it later on if you end up in the same job 20 years from now, when you could have made a potential change for the better? And finally, the last point is that we all slip from time to time, just as I have done. But when you do, kick yourself in the butt, and get right back up and keep on going. I hope this post is helpful to someone.
Decisions
Decisions. We all make them from the time we get out of bed until the end of the day when we go to sleep. Which shirt should I wear to work? What are we going to eat for supper? iPhone or Android? Cable or satellite? Do I drive an extra 5 miles to save a penny a gallon on gas?
For those of us with chronic illness, decisions are even more complex and the stakes are higher. I was pondering this on the way home from my 3 doctor appointments today (my mind never seems to stop, which is probably why I need Trazodone to help me sleep).
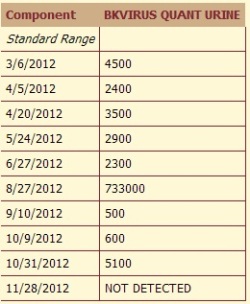
My first 2 appointments today were with the Transplant Surgeon and Transplant Nephrologist. Everything is going well with my kidney. My creatinine is still rock stable at 1.2, and although I again have BK Virus in my urine after 2 negatives, there were only less than 6000 copies in my last urine specimen 2 weeks ago, far below the 2 million copies that my Transplant Surgeon said is the level that he would be “worried” about. It was my last appointment, with the Neuromuscular Neurologist, that got me thinking about the topic of decisions.
As I posted last Spring, I was on Leflunomide, which was used to keep the BK Virus at bay. Not an FDA approved use of the drug, but then again, there IS no standard treatment for BKV. I agreed with the decision by the Surgeon to start Leflumonide. But when my hands were so weak and shaky that I couldn’t get a key into the door, it dawned on me that something was terribly wrong. I figured out that it was not progression of my neuropathy (Charcot Marie Tooth), but rather, was the Leflunomide ravaging my peripheral nerves (and yes, ravaging is an appropriate term). At the time, I phoned my Transplant Coordinator, and was told to stay on Leflunomide, and to see a Neurologist. The referral was made, but 2 months later, I still hadn’t even been contacted about an appointment. As the neurotoxicity worsened, I stopped taking the Leflunomide, and contacted the Transplant Department. The Transplant Coordinator covering for my regular Transplant Coordinator spoke with the doctor, and called me back. When I told her that I stopped the Leflunomide, she asked me if I wanted to lose my kidney. Sheesh, another decision. My first reaction was that she had a helluva lot of nerve putting it that way (I still think that), and being that she is not living with the effects of the med, it wasn’t too professional of her to put it in those terms. Putting the cart before the horse, she continued on by telling me that I may have to receive a last ditch treatment, intravenous Cidofovir, to get rid of the BK virus, since I had stopped the Leflunomide. The problem would be that Cidofovir is VERY toxic to kidneys, and would put my transplant at great risk. Damn, another potential decision. When she went back to the doctor, it turns out the plan was watchful waiting. It obviously turned out well, as my kidney is doing just fine.
Just last Fall, I had a reconstruction done on my right foot. Of the 8 surgeries I’ve had in my life, this was by far THE most painful surgery I have ever had. I was literally screaming in pain when I got to my room after the surgery, but today, for the first time in years, I am walking without a hard plastic orthotic bracing my leg, and my foot is straight. That was a good decision, although during the recovery period, it would have been easy to argue that it wasn’t.
Which brings me to my Neurology visit today. The Neurologist and I had a long talk (my first visit with this doctor), and a good portion of that was on the topic of medications. It turns out that the drug I take to suppress my immune system to prevent my body from rejecting my kidney, Tacrolimus, is a known toxin to peripheral nerves. It’s not likely to cause the damage that the the Leflunomide did, as it’s a “lesser” toxin, but over time, it most likely will cause SOME damage. Risk vs benefit. Progressive damage over decades vs dialysis within months if I don’t take the Tacrolimus and reject my kidney. I’ll take the former. It all boils down to risk vs. benefit.
But being a glass half full kind of guy when it comes to health, there are people far worse off than me. Like the 7 year old local girl who recently lost her life to cancer (Neuroblastoma). Or many of my patients who have disease such as heart failure, cirrhosis, or COPD whose diseases will progress to end stage within a matter of months or several years. I see it every day in my job as a Case Manager.
A doctor will oftentimes make decisions for you – here’s a pill that I’m going to prescribe to help with your blood pressure or cholesterol. A GOOD doctor will explain the risks and the benefits and then ask for your input and decision. Life is full of risks. Too many people today are under the illusion that risks were something we face “in the old day”. Surely, with all of the advancements in science, we shouldn’t have to take risks…. Sorry to burst those people’s bubble, but that’s not the way it works. In fact, with advancements come even MORE risks and more complex decisions. Science and medicine can fix a blockage in the arteries of your heart, and you’ll live longer, as long as you follow the Cardiologist’s instructions. But as we live longer, there is an increased risk that other problems will pop up. And this leads to more decisions.
Unless you are a child, you’ve probably made a decision in the past which you have come to regret. Last year, I had surgery to “tie off” my dialysis fistula. I was told that I would get inflammation in the vein of my upper arm, and it would become red and painful. It did, but when I had a fever of 102, along with the fact that my immune system is suppressed, I made the decision to seek treatment in the Emergency Department (it was a weekend). The doctor decided to admit me to the hospital, and the pharmacist recommended a specific antibiotic. The nurse that was working was a friend of mine, and looked a little nervous when she brought the antibiotic in. It was Vancomycin, which is known for it’s potential to cause kidney damage. Not only that, but the dose was very high-3 grams, followed by 1,750 mg (1.75 grams) every 12 hours after that. I knew it was a high dose, but the facts were that I had a potentially life-threatening infection. Do I risk not treating that and saving my kidney, or risk my kidney to decrease the risk of death or potential problems of an untreated infection? I chose to get the antibiotic, and ended up with Acute Renal Failure from both the med and dehydration. Did I make the right decision? Well, probably not, because they could have used a lower dose or a different antibiotic, but in the end, everything turned out ok, other than the fact that I was in the hospital a few extra days. Hindsight is 20/20. I learned from that one…
Just yesterday, I spoke with the adult child of one of my patients who has had a steady decline in her health over the past year. Her chronic diseases have been well managed up until recently, prolonging both her life and QUALITY of life, but recently, she’s had one problem after another. She made the decision to not get out of bed yesterday, and to not go for her endoscopy today because she has “given up”. She’s not tolerating the medicines that for so long have kept her illnesses at bay; they “come right back up”, probably due to a newly diagnosed disease that may be a result of one of the medicines used to fix an abnormal heart rhythm. Her decision is probably due to her thinking that things just aren’t going to get better no matter what she does, and she’s probably tired of all of the appointments, procedures, and drugs she has to take just to stay alive, and yet still live with her health declining. It’s her decision, and we’ll respect that.
I guess the point of all of this is that if you are faced with a decision, get all of the information you can so that you can make an INFORMED decision, consider risk vs benefit, and don’t beat yourself up when you make a wrong decision.
Latest BK Levels and Foot Fix
From a kidney standpoint, I’ve been doing well. I had 3 negative BK urine tests in a row, but the last one 2 weeks ago was positive for 5800 copies. Not bad, but another negative would have been better.
I still have some residual burning in the fingers from the nerve damage due to the Leflunomide I was on to treat the BK, but I’m off that now, and I can live with it. It’s interesting to note that I never had a negative BK Urine, but once I was off of it, I eventually had 3 in a row. It doesn’t mean anything as it’s anecdotal, but maybe they will do more research on BK to figure out a definitive treatment.
I am a RN Case Manager, and deal with several transplant patients, and a lot of patients with hypertension. I was able to “pick the brain” of a Nephrologist today who specializes in hypertension. I was not aware of this, but Prograf, which is a calcineurin inhibitor, is a potent vasoconstrictor. That means that it causes arteries to get smaller, thus raising blood pressure. Thus, the best antihypertensive choice would be one that causes blood vessels to relax.
I am currently on Lisinopril for my bp, as well as another antihypertensive, Inderal, which is used to treat my hand tremors that worsened after the Leflunomide damaged my peripheral nerves. It’s still not great, but my BP is controlled. I’m going to work on shedding a few pounds, so that should help a lot.
The latest big story is my foot reconstruction.
I had a major foot reconstruction of my right foot in November, and of today, for the first time in many years, can now walk without any orthotic in my shoe.
It’s strange not having my ankle in a fixed position, and I pretty much have to learn to walk normally. I have a tendancy to not flex my ankle, but I know I eventually will be back in the habit of doing this when I walk, based on when I had the other foot reconstructed.
The surgery itself was very painful, and the recovery long (non-weight bearing from Halloween to after New Year’s), and I’ve been in a Bledsoe boot since, but it was well worth it. My foot is very straight now, and although still swollen, it looks great.
I’ve posted x-ray images taken in January, after the surgery, and as you can see, have a lot of hardware.
Foot Reconstruction A Success!
I made it through my 2nd foot reconstruction with flying colors! On November 19, I had a cavovarus foot reconstruction of my right foot, to fix the the deformities caused by Charcot Marie Tooth. As I posted before, a non-healing neuropathic foot ulcer necessitated me having the surgery at this point. I knew I would have to eventually have it, but I was hoping I would have been able to put it off a little longer. However, I’m glad it’s now behind me.
For those familiar with medical “lingo”, the procedures I had done included a Dwyer calcaneal osteotomy, peroneus longus to brevis transfer, first metatarsal losing wedge osteotomy, 5th metatarsal head ex osteotomy, Jones transfer, posterior tib release, toes 2-4 hammertoe corrections.
As you can see from the pics, the surgeon did a LOT of sewing!
I had a similar “reconstruction” done last year, although I didn’t have the hammertoe corrections.
The pain has been manageable this time. Due to the neuropathy, the Anesthesiologist didn’t do a nerve block, but due to excruciating pain (despite a Diluadid infusion/PCA pump), I was taken back to the PACU that night and another Anesthesiologist did 2 nerve blocks, which made the pain tolerable. Now, I’m able to get by with Tylenol and an occasional Tylenol #3.
I’m looking forward to FINALLY getting back to walking. I haven’t been doing any due to the pain from the pressure on the outside of my right foot while in my Ankle Foot Orthosis; there was an extreme amount of pressure on the outside of my foot due to the deformity. I can now get rid of the AFO, and once the cast is off, will be put in a “boot” (Bledsoe?) for a few weeks, and after that, will only need a hard plastic in-the-shoe orthotic insert.
My hemoglobin did drop down to 10.1 post op, but as of last week, I’m back up to 11.8.
As for my kidney transplant status, no “medical misadventures” this time. (here and here)
As you may remember, I had gone off of the Leflunomide back in May, which was used to keep the BK virus suppressed. I had a jump in BK in October from 600 to 5100, and was mildly concerned that it may become a problem, but as of my last check (last week), NO BK! If I’m not mistaken, this is the first that it was negative since April 2009!
I’ve been off CellCept since August 2009, but since my kidney is doing well just on Tacrolimus, the Transplant Surgeon told me that he probably won’t restart the CellCept, even if the BK goes into remission.
I sure hope that I’m done with any medical “speed bumps” for the foreseeable future.
And Yet Another Surgery
I’m headed for another medical first for me: 2 surgeries in 1 year. The first surgery I had this year was when I had my dialysis fistula tied off in April (along with the associated debacle in the hospital several days later).
The previous April, I had surgery on my left foot due to an infection in my foot bone (osteomyelitis) as well as a deep tissue infected from a foot ulcer, and the associated debacle 3 weeks after THAT surgery that put me in to the hospital with Acute Renal Failure from an interaction with my Tacrolimus (I was prescribed Fluconazole for the Candida Parapsilosis in my foot, which caused my Tacrolimus levels to go to 33, leading to ARF).
I just now got back from the Podiatrist, and had the persistent ulcer on my right foot debrided, and given Cipro for the beginning of a cellulitis. It never really healed well from the cellulitis I had last month, and started “acting up” again over the past week. He told me I probably have a multiple organism infection, which if not treated, would most certainly become much more problematic, especially given my immunosuppression.
This is all a direct result of my Charcot Marie Tooth peripheral neuropathy. The muscles in my leg have deteriorated over my 49 years, and although I use a fitted lower leg orthotic, there is a lot of pressure on the outside of my foot, which caused an ulcer. It will never probably heal well, so my Podiatrist suggested I talk to my Orthopaedic surgeon about reconstructive surgery on my right foot. I had it done on my left foot last year, and I’ve had no problems at all on the left since my surgery.
I knew this was coming, and although I’m hesistant to do it, I know I need it, and will have it done.
But, there will be 2 conditions I set before having it done (doctors HATE to hear that).
First and foremost, I will insist on a PCA pump, aka Patient Controlled Analgesia. When I had my left foot done, the Anesthesiologist wouldn’t do a nerve block (rightfully so, being that I have neuropathy). Thus, I ended up getting “bolus” doses of Morphine and Dilaudid, with much nausea/vomiting and poor pain control. They did this because they planned on only an overnight stay, but it ended up that I was in for 2 days. I had PCA for my kidney transplant and gastric bypass, and had excellent control of my pain with little to no nausea.
Second, I will have the Transplant Surgeons consulted while in the hospital to avoid any errors that put my kidney at risk. They are the ones who manage my Tacrolimus, so they will be the ones to ensure that my kidney is safe. After my hospitalization this past April when they gave me too high a dose of Vancomycin, I want somebody watching over the meds I get.
So for now, I’m hoping the Cipro helps, and will hopefully get an appointment to see Dr. Cush within the next several weeks.
As for my readers, feel free to contact me via the comments section. There are people from around the world who read this blog, and I’ve had questions in the past, particularly about BK Virus treatment. Thanks for reading and following. I hope someone finds my posts helpful.
BK Virus Role In Prostate Cancer
A team of Swiss investigators has found a link between the polyomavirus BK and prostate cancer.
It’s an interesting concept. Viruses are well known to be linked to development of cancers. For example, those of us who are immunosuppressed, either purposely through medications, as in the case of transplant or to treat autoimmune diseases, or through disease, such as HIV, are more prone to Lymphoma via Epstein Barr Virus (commonly known to cause mononucleosis).
With more research, there may be the impetus to find a treatment for BKV, given the prevalance of prostate cancer.
As kidney transplant patients are now being screened and monitored for BKV, it will be interesting to see if Prostate Cancer affects male kidney recipients moreso than the general population.
Link via ScienceCodex
Lab Error
I had great news today. Apparently, the last urine BK virus specimen that came back with >700,000 copies. was a lab error. Or, as my transplant coordinator called it, a “fluke”.
I had a repeat urine done on Monday, and there are only 500 copies of virus in my urine. Not 500, 000, but 500. I was diagnosed with BK virus in July, 2009, and at the time, I had greater than 39 MILLION copies in my urine. Since then, it has intermittently been in my blood as well, but my serum BK was negative last week.
So I have to wonder how effective the Leflunomide actually was.
Now, I’ll get my urine checked for BK monthly. That’s a BIG load off of my mind!
I Dodged the Bullet
I had labs a week ago, a serum BK. I’ve found in the past when I’ve had 5 digit BK levels in my urine, I would have it in my blood as well.
However, my serum BK was negative! I had myself all worried about having to go on IV Cidofovir (a nephrotoxic drug), but at this point, I’m not.
I spoke with my Transplant Coordinator Friday, and she told me the good news, and for now, no Cidofovir. She said it’s not unusual to have a high BK level in the urine, and then for it to be much lower the next time. So, to the lab tomorrow to have my urine checked again, and hopefully, it will be down. ‘
I dodged the bullet this time, but IV Cidofovir remains a possibility in the future.
I’ve done some reading, and it’s not known whether the BK comes from the donor, or whether it was in the recipient’s urinary tract.
It’s a virus that usually affects children as a respiratory illness, and my donor was 16 and in a group home. Maybe she had a respiratory infection before she died? I’ll never know, and it’s academic at this point.
Decisions, decisions…..
More speed bumps since my surgery, although unrelated. (speed bump is my turn for a medical issue that I face, deal with, and move on, as opposed to looking at it as a problem that consumes me; it’s all in the approach).
Through the Spring, I had been having a subtle increase in numbness/tingling, tremors, and loss of fine motor skills in my hands. Right after my April hospitalization, it noticeably worsened, to the point where I was having significant burning pain as well, and the one day, I wasn’t even able to get my key into our front door. I racked my brain, and then figured it out. I had a dose increase of my Leflunomide back in January; this is the drug used to treat the BK virus in my transplanted kidney. I looked it up, and sure enough, one of the side effects, although rare, is neurotoxicity. Paired with my existing hereditary peripheral neuropathy, Charcot-Marie-Tooth, this explained my symptoms. I notifed my Transplant Coordinator, and she referred me to a Neurologist but told me to CONTINUE the Leflunomide. The symptoms worsened, though, so I stopped it.
It took 3 months to get in with the Neuromuscular Neurologist, but I finally saw her (for the first time) in mid-August. My suspicions were confirmed-it was the Leflunomide, and the symptoms were mostly irreversible. So she started my on Inderal LA for my hand tremors (my new wonder drug), and did a bunch of labs to check several of my vitamin and mineral levels, all of which were good.
I had my routine transplant labs this past week, and got a call from the Transplant Coordinator; the BK virus level in my urine has skyrocketed since going off of the Leflunomide. In June, the number of BK viral copies in my urine was 2300, and this past week, I have 733,000. They told me to go back on the Leflunomide.
Of course, I refused to do that, given what I went through. I was a bit annoyed when the response to that was “don’t you want to save your kidney?” Yes, of course I do, but I also want to be able to be able to use my hands, so that I can continue to function. While we were talking, she still continued along the same “save your kidney” path, so I finally asked her, for the sake of argument, that if Amoxicillin was effective against BK virus (it isn’t, but Cipro is), and I was allergic to it, would she/the doctor still put me on it? She got my point (I think).
So, she went back to the doctor, and later called me back, telling me that the doctor is “very concerned” (and I’m not?), and he wanted me to get blood work to check for BKV in my blood (I’ve had BKV in my blood before, so I suspect it will be positive), and is considering other treatment.
That treatment would most likely be Cidofovir IV every 2 weeks to try to “clear” me of BKV (which I’ve had for 3 years, albeit controlled prior to this).
The problems are that 1. there is no set treatment for BKV, as it’s discovery has been very recent and 2. IV Cidofovir is potentially toxic to the kidneys.
So it’s come down to this: use of my hands and feet, or saving my kidney.
I’m hoping that I can save my kidney and prevent further damage to my peripheral nerves, and have confidence that I will, but it would be really easy to to let this consume me.
In between all of this, I was in the Emergency Department last month for a foot cellulitis. Every few months, I go to the Podiatrist when needed so that he can pare down the recurring callous I have on the outside of my foot. The callous occurs due to the way I walk-with most of the pressure of each step on the outside of my foot. This is a result of the CMT, which causes gradual loss of nerve conduction, and thus shrinkage of the muscles that keep the foot in a natural position. I wear a padded hard plastic orthotic, but still get a callous. It took a month to get in to the Podiatrist, and 2 days before my appointment, my foot became infected due to an ulcer underneath the callous (much like last year, which led to a bone infection in my other foot and then surgery). However, this time the ulcer was not deep, and it is just about healed now.
So, it’s wait and see for now in regards to the BKV. I hope to blog much sooner to keep you all updated on what happens.